Mandibular Advancement Devices: #1 Snoremate
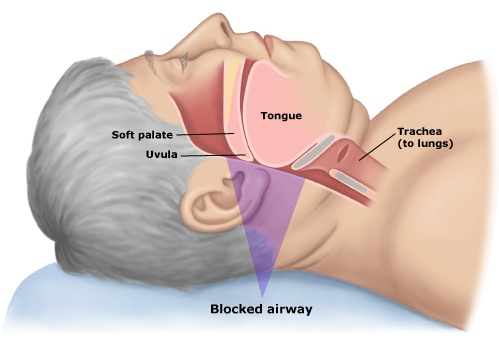
If you've never seen one of these devices before, imagine it as a two gumshields stuck together, with the gumshield for the lower teeth fixed so that it forces the wearer to jut their jaw forward. The mandible is the jawbone, hence the term "Mandibular Advancement"
The idea behind this is that forcing the jaw forward creates more room in the airways by shifting muscles and fat forward slightly, reducing the likliehood and severity of airway obstruction.
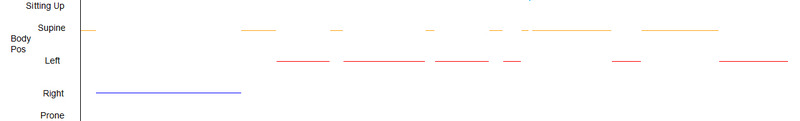
Mandibular advancement (either by a specially made dental device, or by surgery) is a tried and tested concept of reducing snoring and sleep apnoea, so I'm not really putting that to the test, but rather I'm trying out the off the shelf concept, although my snoring is sleep-apnoea related, so unless the device can remedy the apnoea, I doubt that it will affect my snoring.
SnoreMate
This is an off-the-shelf (but custom fit) mandibular advancement device (MAD).
The SnoreMate is made from a thermoplastic that you dip in hot water to make it soft, then bite into it to form a custom fit for your teeth. The SnoreMate can be adjusted by re-dipping it in hot water if you feel the need to advance your lower jaw more to increase the effectiveness of the mouthpiece, something that I did after a few nights of using it.
It was easy to mould, and is the most comfortable of the two mouthpieces that I've tried so far (the other device being the SomnoFit) which I found was too bulky to be comfortable for me). I was surprised that on the first night It stayed in place until around 2am, and on subsequent nights (to get used to it before I monitored it) it remained in place until the morning. It was actually quite easy to get used to. In fact it was surprisingly comfortable, so I purchased a second Snoremate and moulded that one slightly further forward rather than risk losing the comfortable positioning of the first one.
However, there are a couple of drawbacks to the mouthpiece, the main one is saliva build-up! I found myself waking at night just to swallow and clear my mouth. The other drawback is that my gums and a couple of teeth ached for a few of hours in the morning.
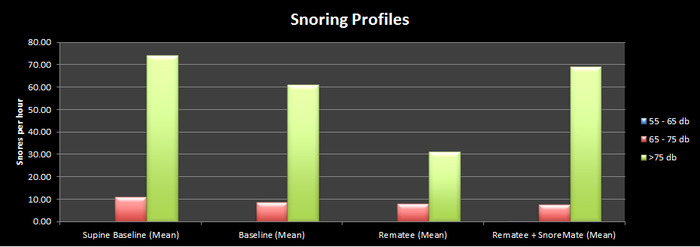
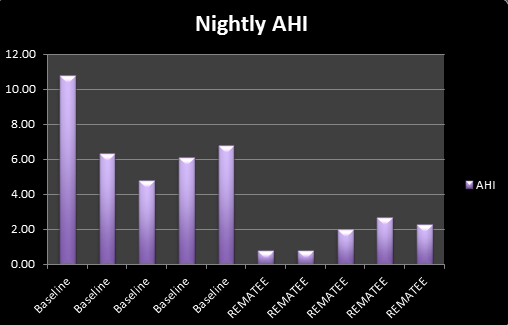
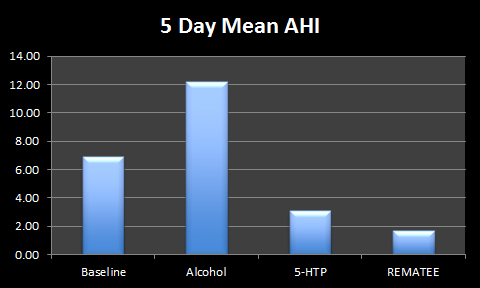
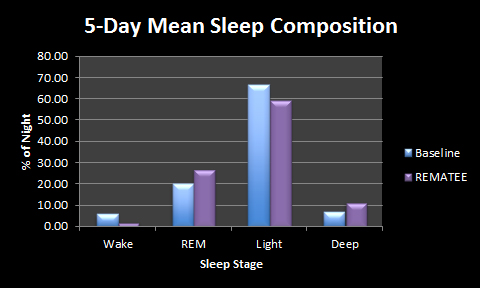
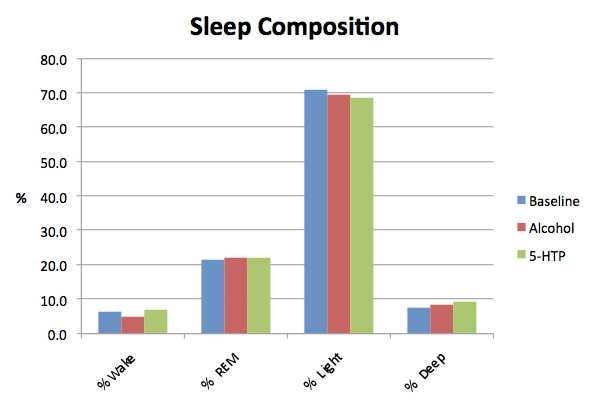
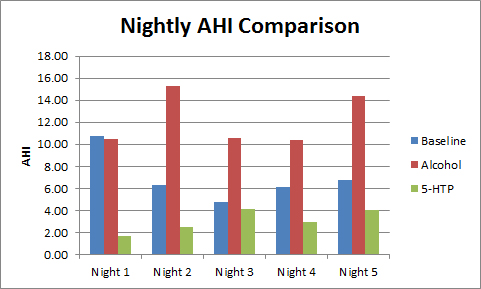
As far as snoring reduction went, using the method explained in this post, I was very surprised. I imagined that everything I used in addition to the Rematee would either improve on the Rematee's effect or make no change. I think that the graph shows why I was surprised...
The SnoreMate actually made my snoring louder! This would have been very annoying for anyone in the house as I managed to reach 98db (about the volume of a drill drilling!). This is an unacceptable volume when you consider that I was already sleeping on my side and wearing a mandibular advancement device. Although to be fair, it is an anti snoring device, and my snoring is more than snoring, it's related to sleep apnoea.
In the following clip it resembled a moose-call.
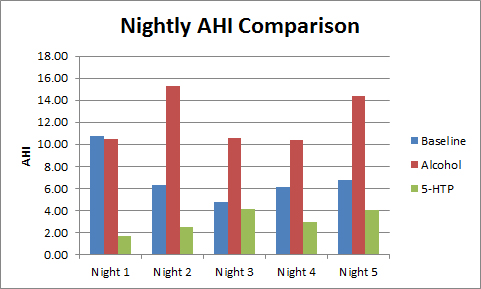
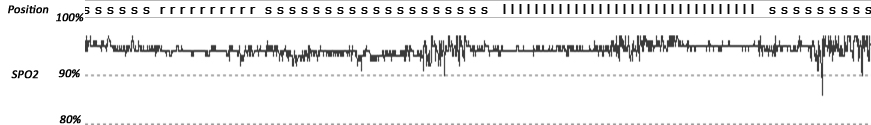
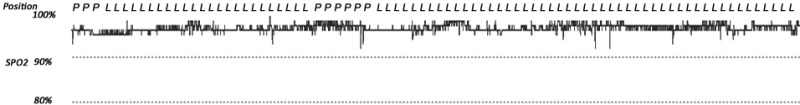
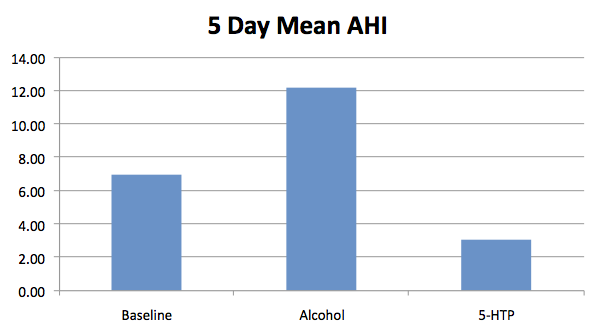
However, I had a lower AHI for the three nights (mean 2.05) with one of the nights using Snoremate with the Rematee giving me my lowest ever AHI of 0.77.
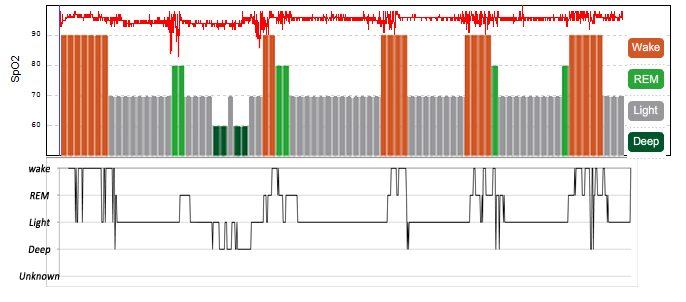
If I had to speculate as to why the snoring increased in volume (and sounded slightly different in tone) yet the AHI was lower, I'd have to say that it was probably due to the fact that, by design, it is impossible to breathe through your mouth with the SnoreMate, so the air has a to take a different path through the nasal passages, rather than through the open mouth of the snorer.
Even wilder speculation: The SnoreMate was probably doing what it was intended to and tightening / stretching the muscles in the airways meaning that they were less prone to relaxing, hence less hypopneas. Again, further speculation, but it is possible that this also caused the snoring to be louder in the same way that in deflating a balloon a screech caused by keeping the neck taut is louder and higher pitched that if you were to let the neck relax causing a quieter lower-tone rapserry sound.
I was so intrigued by this hint that it was working, that I've made an appointment at my dentist to have a professional Mandibular Advancement Device constructed for me and I'm looking forward to being able to compare the results. My hope is that the professional device will allow me to further advance my jaw, keeping my airway muscles even tighter, elimating my apnoeas and maybe my hypopneas (and hopefully snoring too).
 MAD,
MAD,  Mandibular Advancement Device,
Mandibular Advancement Device,  apnoea | in
apnoea | in  Apnoea,
Apnoea,  Experiment
Experiment